How to Order ? Simple.
-

1.
Select Treatment
Choose from our treatment options or speak to the in-store pharmacist for advice
-

2.
Complete Medical Questionnaire
Complete our free online medical consultation to be reviewed by our Clinical Team
-

3.
Collect Medication from Local Pharmacy
We will notify you when your medication is ready for collection
Advice for Nasal Infection
These infections can be caused by factors such as trauma or injury from nose-picking, excessive nose blowing, or nasal piercings, which create opportunities for bacteria to enter. Preexisting conditions like allergies and dermatitis can also make the area more susceptible to infection, along with poor hygiene practices or exposure to contaminated environments.
Common bacteria involved in these infections include Staphylococcus aureus, which is often found on the skin, as well as Streptococcus species and, in some cases, Haemophilus influenzae. Symptoms typically include redness and swelling around the nostrils, pain or tenderness in the affected area, crusting or discharge that may be yellow or green, itching or irritation, and sometimes bleeding due to irritation. More severe infections can lead to systemic symptoms such as fever and malaise.
Diagnosis generally involves a review of the medical history, a physical examination by a healthcare provider, and, in some cases, culture tests to identify the specific bacteria responsible for the infection. Treatment usually includes topical antibiotics applied to the affected area, oral antibiotics for more extensive infections, and over-the-counter pain relievers to alleviate discomfort. Maintaining good hygiene practices is also essential.
Home care strategies can help manage symptoms effectively. These include gently cleaning the affected area with saline solutions and applying warm compresses to reduce pain and promote healing. Preventive measures involve maintaining good personal hygiene, avoiding nose-picking, and addressing allergic or skin conditions to prevent irritation.
Individuals should seek medical attention if they experience severe or worsening symptoms, persistent pain or swelling, or signs of systemic infection, such as a high fever. Recognizing the signs of nasal bacterial infections in the nostrils is crucial for prompt treatment and effective recovery. For personalized medical advice, consulting a healthcare professional is recommended.
The nasal bacterial infections of the nostrils can vary based on the severity of the infection and the specific bacteria involved. Here’s a detailed look at the common symptoms associated with these infections:
Localized Symptoms
1. Redness and Swelling:
- The skin around the nostrils may appear red and swollen due to inflammation.
- This can extend into the nasal vestibule, leading to noticeable changes in appearance.
2. Pain or Tenderness:
- Individuals often experience localized pain or tenderness in and around the nostrils.
- Touching or pressing on the area might exacerbate the discomfort.
3. Discharge:
- There may be a thick discharge from the nostrils, which could be yellow, green, or even pus-like in consistency, indicating an active infection.
- The discharge may crust around the nostrils, leading to additional irritation.
4. Crusting:
- Crusts may form inside and around the nostrils due to dried discharge.
- This can lead to discomfort and may cause further irritation if removed improperly.
5. Bleeding:
- Some individuals may experience minor bleeding, particularly if the area is frequently irritated by nose-picking or excessive blowing.
- Blood may be mixed with discharge or appear separately.
Systemic Symptoms
While nasal bacterial infections typically manifest localized symptoms, they can also lead to systemic symptoms, particularly if the infection spreads or becomes more severe:
6. Fever:
A mild to moderate fever may develop as the body responds to the bacterial infection. Fever can indicate that the infection is more severe or systemic.
7. Fatigue and Malaise:
Individuals may feel unusually tired or weak as the body fights off the infection. A general sense of malaise or discomfort may accompany this fatigue.
8. Headache:
- The inflammation and pressure in the nasal area can lead to headaches, particularly if sinus involvement occurs.
- Pain may be felt in the forehead, cheeks, or temples and can worsen when bending over.
9. Ear Pain or Pressure:
- Infections can lead to pressure changes affecting the ears, resulting in discomfort or a feeling of fullness.
- This happens due to the interconnectedness of the nasal passages, sinuses, and Eustachian tubes.
Other Symptoms
10. Itching or Irritation:
- Affected individuals may experience itching around the nostrils, which can lead to additional irritation if scratched or picked at.
- Irritation may stem from friction against clothing or fingers, as well as from drying secretions.
11. Sore Throat:
- Postnasal drip from the infected nostrils can cause a sore throat due to mucus drip irritation.
- This may present as a scratchy or painful sensation in the throat.
12. Halitosis (Bad Breath):
- An infection can lead to less pleasant breath odors due to the presence of bacteria and discharge.
- This can be particularly noticeable if one has nasal congestion or drainage issues.
Severity Signs
In more severe cases, symptoms may escalate, and individuals should seek prompt medical attention if they experience:
- Worsening facial swelling or pain.
- Severe headache or pressure that is not relieved with over-the-counter medications.
- High fever (greater than 101°F or 38.3°C).
- Signs of systemic infection, such as chills or a rapid heartbeat.
Recognizing these symptoms early can help in obtaining timely treatment, reducing the risk of complications associated with bacterial nasal infections. For any persistent or concerning symptoms, consultation with a healthcare professional is essential for appropriate evaluation and management.
Nasal bacterial infections of the nostrils can occur due to a variety of factors. Here are the primary causes:
1. Trauma or Injury
- Nose Picking: Frequent or aggressive nose-picking can create small abrasions in the skin, allowing bacteria to enter and cause infection.
- Nasal Piercings: Piercing the nostrils can introduce bacteria into the area, leading to potential infections.
- Excessive Blowing: Forcibly blowing the nose can irritate the skin and mucous membranes, increasing the risk of infection.
2. Pre Existing Conditions
- Allergies: Allergic reactions can cause inflammation and swelling of the nasal passages, making them more susceptible to bacterial invasion.
- Dermatitis: Skin conditions such as eczema, which may affect the nasal area, can compromise the skin barrier and promote bacterial entry.
- Chronic Sinusitis: Individuals with chronic sinusitis may have recurrent bacterial infections, as the condition can create an environment favorable for bacterial growth.
3. Infection Following a Viral Illness
- Viral Upper Respiratory Infections: Viral infections, such as the common cold, can precede bacterial infections by causing nasal congestion and inflammation, interfering with normal mucus drainage and allowing bacteria to proliferate.
4. Hygiene Practices
- Poor Hygiene: Inadequate hand hygiene or not cleaning the nasal area properly can lead to bacterial colonization.
- Contaminated Objects: Touching the nostrils with contaminated hands or items, such as tissues or towels, can introduce bacteria into the nasal vestibule.
5. Environmental Factors
- Pollution and Irritants: Exposure to environmental irritants, such as smoke, strong perfumes, or chemical fumes, can irritate the nasal passages, making them more susceptible to infection.
- Dry Air: Dry air, especially during winter months or in artificially heated environments, can cause dryness and cracking of the nasal tissues, increasing the risk of infection.
6. Immune System Factors
- Weakened Immune System: Individuals with compromised immune systems or those taking immunosuppressive medications are at a higher risk for infections, including bacterial nasal infections.
- Chronic Illnesses: Conditions such as diabetes or HIV can affect immune response, making infections more likely.
7. Bacterial Colonization
- Normal Flora Overgrowth: Certain bacteria, which are normally present on the skin, can overgrow due to various factors and cause infection in the nasal vestibule.
- Bacterial Contamination from Other Body Areas: Bacteria from other areas, such as oral or dental infections, can be introduced to the nasal area.
- Recognizing these causes can help in adopting preventive measures to reduce the risk of nasal bacterial infections. Maintaining good hygiene, limiting trauma to the nostrils, and addressing underlying health conditions are important steps in prevention. For any concerning symptoms or frequent infections, consulting a healthcare professional is advisable.
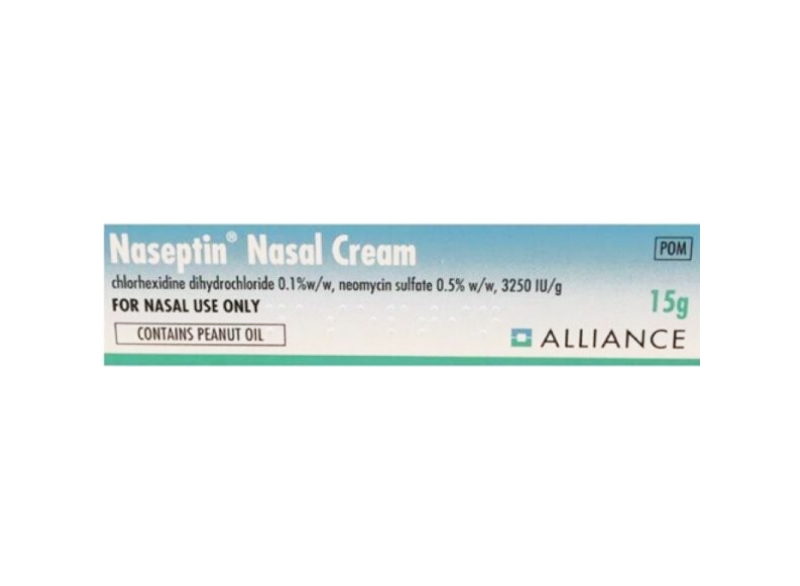
At Pharmacinta, we provide topical antibiotics that are commonly prescribed to treat bacterial infections of the nostrils, particularly in cases such as nasal vestibulitis. Bactroban and Naseptin are one of the most frequently used topical antibiotics for this purpose, as it effectively targets Staphylococcus aureus and other bacteria. When using a topical antibiotic, it is important to first clean the affected area with mild soap and water to reduce the risk of further irritation or infection.
After patting the area dry, a thin layer of the antibiotic ointment should be applied directly to the infected nostril and surrounding skin using a clean fingertip or cotton swab. Healthcare providers typically recommend applying the antibiotic two to three times daily for up to 10 days, depending on the severity of the infection and the specific product used. It is essential to follow the prescribed duration of treatment to ensure the infection is fully resolved and to prevent the development of antibiotic resistance.
Patients should monitor for any signs of improvement or worsening symptoms during treatment. If the infection does not improve within a few days or if there are signs of an adverse reaction, such as increased redness or swelling, it is important to consult a healthcare professional for further evaluation. Overall, topical antibiotics can provide effective localized treatment for bacterial nasal infections when used correctly.
In addition to topical antibiotics, there are several alternative treatments that may help manage bacterial nasal infections of the nostrils. These alternatives can complement standard treatments or be used in specific cases where antibiotics may not be necessary. Here are some alternative treatment options:
1. Saline Nasal Sprays or Rinses
- Saline Solutions: Using saline sprays or rinses can help cleanse the nasal passages and reduce mucus buildup.
- Benefits: They help moisturize the nasal membranes, flush out irritants, and decrease congestion, creating an environment less conducive to bacterial growth.
2. Warm Compresses
- Application: Applying a warm compress to the affected area can help reduce pain and swelling.
- Benefits: The warmth improves blood circulation and promotes drainage of any clogged mucus, aiding in the healing process.
3. Over-the-Counter Pain Relievers
- NSAIDs and Acetaminophen: Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or acetaminophen can alleviate pain and reduce inflammation.
- Use: These medications can help manage discomfort associated with nasal infections.
4. Topical Antiseptics
- Antiseptic Ointments: Products containing antiseptics, such as hydrogen peroxide or tea tree oil, may be applied to the affected area to help cleanse it and reduce bacterial load.
- Caution: It’s important to use these with caution, as they can irritate sensitive skin.
5. Humidifiers
- Use in Living Spaces: Using a humidifier can add moisture to the air, helping to soothe dry nasal passages and reduce irritation.
- Benefits: Increased humidity can help alleviate symptoms caused by dry air and promote healing.
6. Vitamin Supplements and Nutritional Support
- Vitamins C and D: Supporting the immune system with vitamins, such as vitamin C and D, may help the body fight infections more effectively.
- Zinc: Some studies suggest that zinc may help reduce the duration of respiratory infections.
7. Herbal Remedies
- Echinacea and Goldenseal: These herbs are sometimes used to boost the immune system and may have mild antibacterial properties.
- Caution: Consult with a healthcare professional before starting any herbal remedies, as they can interact with medications.
8. Avoiding Irritants
- Environmental Modifications: Avoiding smoke, strong fragrances, and other environmental irritants can reduce nasal irritation and the risk of aggravating infections.
- Allergen Management: Managing allergies is essential, as they can lead to nasal inflammation and make infections more likely.
9. Lifestyle Changes
- Hydration: Staying well-hydrated helps maintain mucus flow and support overall immune function.
- Rest: Adequate rest and sleep are important for the body’s recovery process when dealing with any infection.
10. Consultation with a Specialist
- ENT Specialist: In cases of recurrent infections or chronic issues, consulting an Ear, Nose, and Throat (ENT) specialist may provide additional treatment options, including surgical interventions if necessary.
Using these alternative treatment options can help manage symptoms and support the natural healing process of bacterial nasal infections. However, it’s essential to consult a healthcare professional before starting any new treatment to ensure it is appropriate for your specific situation and to discuss any potential interactions with existing medications.
Frequently Asked Questions
Nasal infections refer to inflammatory conditions affecting the nasal passages, often caused by viruses, bacteria, or fungi. Common types include sinusitis (sinus infections) and rhinitis (inflammation of the nasal lining).
Treatment options vary based on the cause. For viral infections, supportive care is generally recommended, including rest, hydration, and over-the-counter medications. If a bacterial infection is present, antibiotics may be prescribed. Allergic rhinitis can be treated with antihistamines or nasal corticosteroids, while chronic sinusitis may require additional treatments, including surgery in severe cases.
Prevention strategies include washing hands frequently, avoiding close contact with sick individuals, effectively managing allergies, not smoking and avoiding secondhand smoke, and using a humidifier to maintain nasal moisture during dry seasons.
Consult a doctor if symptoms persist for more than 10 days, worsen after initial improvement, or if you experience severe headache or facial pain. Additionally, seek medical attention for high fever, swelling around the eyes, or any breathing difficulties.
Some nasal infections, particularly those caused by viruses (like the common cold), can be contagious. Bacterial sinus infections are less likely to be contagious.
Yes, complications can occur, including chronic sinusitis, nasal polyps, and, in rare but serious cases, infections that spread to the eyes or brain.
Effective home remedies include steam inhalation to help relieve congestion, saline nasal sprays or rinses to clear mucus and allergens, warm compresses applied to the face for pain relief, herbal teas, and broths for hydration and soothing effects. Humidifiers can be beneficial by adding moisture to the air, which helps keep nasal passages moist and eases breathing.
Incorporating lifestyle changes such as lowering stress levels, maintaining a healthy diet rich in vitamins and minerals (especially vitamin C and zinc), engaging in regular physical activity, and ensuring adequate sleep can help strengthen the immune system. Additionally, avoiding allergens and irritants can reduce the likelihood of developing nasal infections.
Nasal infections can recur, particularly for individuals with underlying conditions such as allergies or anatomical issues affecting sinus drainage. If recurrent nasal infections occur, it’s important to discuss this with a healthcare provider who may recommend further evaluation and potential preventive measures, such as allergy testing or treatment options for underlying conditions.
Topical antibiotics are medications applied directly to the skin or mucous membranes to treat localized infections. They work by preventing the growth of bacteria and are often used for skin infections, wounds, and some nasal infections.
Topical antibiotics may be prescribed for nasal infections when there is localized bacterial infection, such as in cases of persistent nasal vestibulitis (infection of the skin at the entrance of the nostrils) or in conjunction with other treatments for sinusitis, particularly if there is a suspicion of bacterial involvement.
The benefits of using topical antibiotics include localized treatment that minimizes systemic exposure, leading to fewer side effects. They can effectively treat localized infections, reduce bacterial load in the nasal passages, and may assist in preventing the progression of infection to more severe forms.
Though generally safe, topical antibiotics can cause side effects in some individuals. Potential side effects may include local irritation, burning sensations, or allergic reactions. Prolonged use can lead to antibiotic resistance or imbalance in normal nasal flora. It’s essential to follow healthcare provider recommendations to minimize risks.
The duration of treatment will depend on the specific infection and the healthcare provider’s recommendations. Typically, treatment may last from several days to a couple of weeks. It's crucial to follow the prescribed course even if symptoms improve to prevent recurrence or resistance.
Yes, topical antibiotics may be used alongside other treatments. For instance, they can be part of a comprehensive management plan for sinusitis, where other medications (like oral antibiotics, nasal corticosteroids, and saline rinses) may also be prescribed to address inflammation and improve drainage.
Yes, available alternatives include oral antibiotics for more widespread bacterial infections, nasal corticosteroids to reduce inflammation, saline nasal irrigation for cleansing nasal passages, and even antifungal medications if a fungal infection is suspected. Treatment options should be tailored to the individual’s specific condition, and discussing solutions with a healthcare provider is always recommended.
Preventive measures might include maintaining good nasal hygiene through regular saline rinsing, avoiding allergens and irritants, managing underlying conditions (such as allergies), practicing frequent handwashing, and staying away from close contact with individuals who have respiratory infections.