How to Order ? Simple.
-

1.
Select Treatment
Choose from our treatment options or speak to the in-store pharmacist for advice
-

2.
Complete Medical Questionnaire
Complete our free online medical consultation to be reviewed by our Clinical Team
-

3.
Collect Medication from Local Pharmacy
We will notify you when your medication is ready for collection
Advice for Infected Insect Bite
Insect bites tend to be seasonal and increase during the summer months when more insects are active and more skin is exposed. Studies suggest that 56-94% of people are stung by insects such as bees, wasps or ants, at least once in their lifetime. In the UK, insect stings are the second most common cause of anaphylaxis outside of medical settings.
Insect venom induces a toxic reaction at the site of the sting. Large local reactions are due to allergy. In the UK, wasp venom allergy is more common than bee venom allergy, and biting insects rarely cause systemic reactions.
A German study found that large local reactions occurred in up to 25% of the population, and as many as 3.5% develop IgE-mediated, potentially life-threatening anaphylaxis, of which about 20 people die in Germany each year.
The cause of a bite can often be readily diagnosed where an insect remains attached, as in ticks (small blood-sucking bugs often thought of as insects) and with bloodsuckers that are highly visible - eg, mosquitoes, midges and black flies. Others may not be so easy to diagnose because they bite at night or when the patient is asleep - eg, some mosquitoes, sandflies, bedbugs and triatomine bugs, or when it is inconspicuous and does not cause an immediately painful bite - eg, harvest mites, some fleas and biting flies. Bites typically result in single or grouped pruritic erythematous papules. Some may have a central punctum and others may be bullous.
Risk Factors
Weakened Immune System: Individuals with compromised immune systems, such as those with HIV/AIDS, undergoing chemotherapy, or taking immunosuppressive drugs, are more prone to infections.
Pre-existing Skin Conditions: Conditions like eczema, psoriasis, or open wounds can increase susceptibility to infections.
Poor Hygiene: Not keeping the bite area clean can allow bacteria to proliferate and cause infection.
Complications
Cellulitis: This is a serious bacterial skin infection that can spread rapidly if not treated promptly. It typically involves deeper layers of the skin and subcutaneous tissues.
Sepsis: Sepsis is a life-threatening condition caused by the body’s response to an infection. It can lead to tissue damage, organ failure, and death if not treated immediately.
Abscess Formation: A painful collection of pus, known as an abscess, can form under the skin. This may require drainage by a healthcare professional.
Localized Symptoms
Redness and Swelling: The area surrounding the bite becomes red and swollen, which is a common sign of inflammation. This reaction is part of the body's immune response to any infection or foreign material.
Warmth: The infected area often feels warm to the touch due to increased blood flow as the body tries to fight off the infection.
Pain and Tenderness: The bite site may become increasingly painful or tender. This discomfort can range from mild to severe, depending on the extent of the infection.
Pus or Discharge: The presence of yellow or green pus indicates a bacterial infection. The discharge may also have an unpleasant odor.
Itching: Persistent itching is common, though it can become more intense and problematic when an infection is present. Scratching can worsen the situation by further irritating the skin and potentially spreading the infection.
Blistering: Blisters filled with fluid may form around the bite. These can burst and lead to further skin irritation and infection if not properly managed.
Systemic Symptoms
Fever and Chills: A high fever accompanied by chills can indicate that the infection is spreading beyond the localized area, signaling a more serious condition.
Swollen Lymph Nodes: Lymph nodes near the infected area (e.g., in the armpits or groin) may swell as they work to filter out harmful pathogens.
Fatigue: General tiredness and a feeling of malaise can occur as the body uses more energy to fight the infection.
Nausea or Headache: These symptoms might develop if the infection is more severe or systemic, affecting the whole body rather than just the bite area.
Infected insect bites occur when bacteria or other pathogens enter the body through the bite wound. Reasons for the bite to become infected can include:
Bacterial Entry: Bacteria such as Staphylococcus aureus or Streptococcus pyogenes can enter the body through the bite wound. These bacteria are commonly found on the skin and in the environment.
Scratching: Scratching the bite can break the skin further, providing an entry point for bacteria. This is a common way infections start, as the initial itchiness from the bite often leads to scratching.
Insect Saliva: Some insect bites introduce pathogens directly through their saliva. For instance, ticks can transmit Lyme disease, and mosquitoes can transmit malaria.
When an insect bite becomes infected, antibiotic treatment may be necessary to eliminate the infection and prevent complications. Depending on the severity of the infection and the suspected or confirmed bacteria, different antibiotics may be prescribed.
At Pharmacinta, we provide the following antibacterial treatment for infected insect bites:
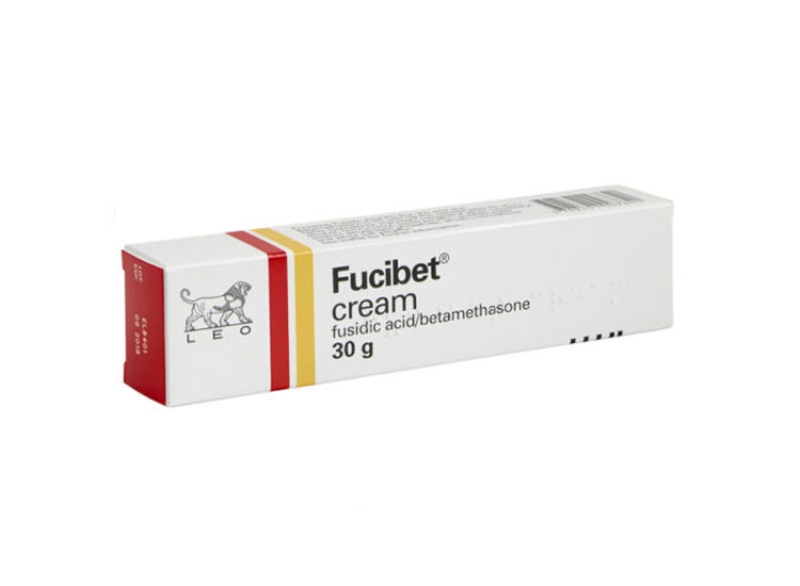
- Topical Antibiotics: For mild infections, topical antibiotic creams and ointments like Fucidin or Fucidin HC can be applied to the bite. Topical antibiotics are usually applied 2-3 times a day after cleaning the bite area. They are suitable for minor infections and can help prevent the progression of the infection.
- Oral Antibiotics: If the bite becomes significantly infected, our clinician may prescribe oral antibiotics to treat the infection. Our clinicians may prescribe antibiotics including Flucloxacillin and Clarithromycin. Oral antibiotics are typically prescribed for 7-14 days, depending on the severity of the infection and the specific antibiotic used. It is crucial to complete the entire course of antibiotics, even if symptoms improve, to ensure the infection is fully eradicated.
What to do if you've been bitten or stung
To treat an insect bite or sting:
- Remove the sting or tick if it's still in the skin
- Wash the affected area with soap and water
- Apply a cold compress (such as a flannel or cloth cooled with cold water) or an ice pack to any swelling for at least 10 minutes
- Raise or elevate the affected area if possible, as this can help reduce swelling
- Avoid scratching the area, to reduce the risk of infection
- Avoid traditional home remedies, such as vinegar and bicarbonate of soda, as they're unlikely to help
When to get medical advice
Contact your GP or Pharmacinta if:
- You're worried about a bite or sting
- Your symptoms do not start to improve within a few days or are getting worse
- You've been stung or bitten in your mouth or throat, or near your eyes
- A large area (around 10cm or more patch of skin) around the bite becomes red and swollen
- You have symptoms of a wound infection, such as pus or increasing pain, swelling or redness
- You have symptoms of a more widespread infection, such as a high temperature, swollen glands and other flu-like symptoms
When to get emergency medical help
Dial 999 for an ambulance immediately if you or someone else has symptoms of a severe reaction, such as:
- Wheezing or difficulty breathing
- A swollen face, mouth or throat
- Feeling sick or being sick
- A fast heart rate
- Dizziness or feeling faint
- Difficulty swallowing
- Loss of consciousness
- Emergency treatment in hospital is needed in these cases.
Initial First Aid
Wash the Area: Clean the bite area with soap and water to remove any bacteria or irritants.
Cold Compress: Apply a cold compress or ice pack wrapped in a cloth to reduce swelling and numb the area, providing relief from pain and itching.
Topical Treatments
Antiseptic Creams: Over-the-counter antiseptic creams or ointments can help prevent infection.
Hydrocortisone Cream: This steroid cream can reduce inflammation, itching, and redness.
Calamine Lotion: Helps soothe itching and irritation.
Antihistamine Creams: Products containing diphenhydramine can help reduce itching and allergic reactions.
Oral Medications
Antihistamines: Oral antihistamines like cetirizine can help reduce itching and allergic reactions.
Pain Relievers: Over-the-counter pain relievers such as ibuprofen can help manage pain and reduce inflammation.
Herbal Remedies
Aloe Vera: Known for its soothing properties, aloe vera gel can reduce inflammation and itching.
Calendula: This herb has anti-inflammatory and antimicrobial properties. Applying calendula cream or ointment can help soothe the skin.
Tea Tree Oil: It has antiseptic and anti-inflammatory properties. Dilute a few drops in a carrier oil and apply to the bite.
Witch Hazel: Acts as an astringent, reducing swelling and irritation.
Essential Oils
Lavender Oil: Known for its calming and anti-inflammatory properties, lavender oil can be applied directly to the bite.
Peppermint Oil: Provides a cooling sensation and helps reduce itching. It should be diluted before application.
Home Remedies
Baking Soda Paste: A paste made from baking soda and water can help neutralize the itch and reduce swelling.
Apple Cider Vinegar: Applying diluted apple cider vinegar can help with itching and inflammation due to its antibacterial properties.
Honey: Raw honey has antibacterial and anti-inflammatory properties and can be applied directly to the bite.
Hydrotherapy
Cold Compress: Applying a cold compress or an ice pack wrapped in a cloth can reduce swelling and numb the area, providing relief from pain and itching.
Dietary Supplements
Vitamin C: Known for its immune-boosting properties, vitamin C can help reduce inflammation and promote healing.
Zinc: This mineral supports immune function and can help the skin heal faster.
Lifestyle and Preventive Measures
Proper Hygiene: Keeping the bite area clean and dry to prevent further infection.
Avoid Scratching: Scratching can introduce bacteria and worsen the infection.
Protective Clothing: Wearing long sleeves and pants in areas with many insects can prevent bites.
Insect Repellent: Using natural insect repellents like citronella or eucalyptus oil can help prevent bites.
Frequently Asked Questions
An infected insect bite occurs when bacteria enter the skin through a bite, leading to redness, swelling, and pus.
Look for increased redness, warmth, swelling, pain, pus, or systemic symptoms like fever.
Clean the area, apply a cold compress, and avoid scratching. Seek medical advice if symptoms worsen.
If you experience signs of an allergic reaction, such as severe swelling, difficulty breathing, or widespread rash, seek immediate medical attention. You may need emergency treatment, including antihistamines or corticosteroids.
While some home remedies can provide relief, it's important to consult a healthcare professional for proper diagnosis and treatment, especially if infection is suspected. Home remedies may complement treatment but should not replace medical advice.
With appropriate treatment, mild infections often start to improve within a few days. More severe infections may take longer to heal. Always follow your healthcare provider's instructions for the best recovery outcome.
Common insects that can lead to infected bites include: - Mosquitoes - Bees and wasps - Ants - Fleas - Ticks - Spiders - Horseflies
Yes, if left untreated, an infection from a bite can spread to surrounding tissues or enter the bloodstream, leading to more serious conditions like cellulitis or sepsis.
Healing time can vary based on the severity of the infection and treatment. Mild infections may heal within a few days to a week, while more severe infections could take longer, possibly requiring two weeks or more.
Yes, individuals at higher risk include: - Those with weakened immune systems (e.g., due to diabetes, HIV, or cancer treatments). - People with chronic skin conditions (e.g., eczema or psoriasis). - Children and the elderly, who may have more delicate skin.
Signs of worsening infection include: - Increasing redness and swelling around the bite. - Development of a painful lump or abscess. - Presence of red streaks radiating from the bite site. - Fever or chills developing after the bite.
No, always wrap ice or a cold pack in a cloth or towel to prevent frostbite and skin damage. Apply it for 15-20 minutes at a time.
Yes, it is crucial to complete the entire course of antibiotics as prescribed to ensure that the infection is fully eradicated and to prevent antibiotic resistance.
Yes, over-the-counter antihistamines like diphenhydramine (Benadryl) or cetirizine (Zyrtec) can help alleviate itching and swelling from allergic reactions to insect bites.
If you miss a dose, take it as soon as you remember. If itís close to the time for your next dose, skip the missed dose and continue with your regular schedule. Never double up on doses without consulting a healthcare provider.
Some natural remedies include: - Aloe Vera: Soothes inflammation. - Honey: Has antibacterial properties. - Baking Soda Paste: Helps reduce itching and irritation.
In rare cases, if an infection is severe or improperly treated, it can lead to chronic issues, such as recurrent infections or scarring.
A normal bite typically shows mild redness and slight swelling. In contrast, an infected bite exhibits significant inflammation, warmth, pain, pus, and possibly systemic symptoms like fever.
To relieve itching, you can: - Apply a cold compress. - Use anti-itch creams (like hydrocortisone). - Take an oral antihistamine. - Apply baking soda paste or calamine lotion.
While itís difficult to prevent all insect bites, you can minimize the risk by using insect repellents, wearing protective clothing, and avoiding areas with high insect activity, especially during peak times.
Fucidin Cream is primarily used to treat bacterial skin infections, such as impetigo, infected wounds, and infected insect bites. It contains fusidic acid, which is effective against specific bacteria.
Fucidin H Cream combines fusidic acid with hydrocortisone. It is used to treat inflammatory skin conditions that are infected or at risk of infection, providing both antibacterial and anti-inflammatory effects.
Fucidin H Cream is generally safe for children, but itís essential to consult a healthcare provider for appropriate use and dosage.
Fucidin Cream can be used on the face for bacterial infections, while Fucidin H Cream should be used cautiously and under medical advice due to the presence of hydrocortisone.
Follow your healthcare provider's advice regarding duration. Generally, these creams should not be used for extended periods to avoid potential skin thinning or resistance.
Yes, you can cover the area with a bandage unless otherwise instructed by your doctor. Ensure the area is clean and dry before applying.
If you miss a dose, apply it as soon as you remember. If it's almost time for the next dose, skip the missed dose and continue with your regular schedule.
No, Fucidin Cream is not effective against fungal infections. It is specifically designed for bacterial infections. Consult a healthcare provider for fungal treatments.
Fucidin H Cream can be used on minor open wounds, but itís essential to consult a healthcare provider for proper guidance based on the wound's severity.
Consult your doctor or pharmacist before combining with other topical medications to avoid interactions or increased irritation.
If symptoms do not improve within a few days of using the cream or worsen, consult your healthcare provider for further evaluation and possible alternative treatment.
Avoid using on large areas of skin, and do not apply to broken or eczema-affected skin without medical advice. Use only for the prescribed duration to prevent resistance or side effects.
Consult your healthcare provider before using these creams during pregnancy to assess the benefits and risks for both the mother and baby.
Clarithromycin works by binding to the bacterial ribosome, inhibiting protein synthesis. This action prevents the bacteria from growing and reproducing, leading to the elimination of the infection.
No, clarithromycin is a prescription medication and must be prescribed by a healthcare provider.
Clarithromycin is generally effective for respiratory infections caused by susceptible bacteria, including those causing bronchitis and pneumonia.
Yes, clarithromycin is part of combination therapy to treat Helicobacter pylori infections, which can cause stomach ulcers.
If you are pregnant or breastfeeding, discuss the potential risks and benefits with your doctor. Clarithromycin should be used during pregnancy or breastfeeding only if clearly needed and prescribed by a healthcare provider.
No, clarithromycin is an antibiotic and is not effective against viral infections such as the flu or the common cold.
If you suspect an overdose, seek immediate medical attention or call a poison control center. Symptoms of overdose may include severe nausea, vomiting, diarrhea, and abdominal pain.
Yes, clarithromycin can cause allergic reactions in some individuals. Symptoms may include rash, itching, swelling, severe dizziness, and difficulty breathing. Seek immediate medical attention if you experience these symptoms.
It is advisable to avoid alcohol while taking clarithromycin as it can increase the risk of liver damage and exacerbate side effects like dizziness and gastrointestinal discomfort.
If your symptoms do not improve or worsen after a few days of treatment, contact your healthcare provider for further evaluation and possible adjustment of your treatment plan.
Flucloxacillin is an antibiotic used to treat bacterial infections, particularly those caused by Staphylococcus aureus and other Gram-positive bacteria. Common conditions include skin infections, respiratory tract infections, and bone infections.
Flucloxacillin works by inhibiting bacterial cell wall synthesis, effectively killing the bacteria and stopping the infection from spreading.
Yes, Flucloxacillin can be used in children, but the dosage will be adjusted based on the child's age and weight. Consult a pediatrician for proper dosing.
While thereís no direct contraindication, it's generally advisable to limit alcohol consumption while on antibiotics to avoid potential stomach upset and dehydration.
Flucloxacillin is generally considered safe during pregnancy, but consult your healthcare provider to assess the risks and benefits based on your specific situation.
Complete the full course of Flucloxacillin as prescribed, even if you start feeling better before finishing the medication. This helps prevent antibiotic resistance.
If you miss a dose, take it as soon as you remember. If it's close to the time for your next dose, skip the missed dose and continue with your regular schedule. Do not double up.
Yes, Flucloxacillin can interact with certain medications, including anticoagulants and other antibiotics. Always inform your doctor about all medications you are taking.
If symptoms do not improve within a few days or worsen while taking Flucloxacillin, contact your healthcare provider for further evaluation and possible alternative treatment.
There are no specific dietary restrictions, but it is generally recommended to take the medication on an empty stomach for better absorption.
No, Flucloxacillin is ineffective against viral infections. It is specifically designed to target bacterial infections.
No, you should complete the entire prescribed course of Flucloxacillin, even if you feel better, to ensure the infection is fully treated and to prevent resistance.
If you suspect an overdose, seek immediate medical attention or contact your local poison control center. Symptoms may include severe gastrointestinal upset or allergic reactions.
Flucloxacillin is not effective against methicillin-resistant Staphylococcus aureus (MRSA). Other antibiotics are required for MRSA infections.